
Resistance was not due to β-lactamase production but due to the expression of an additional penicillin-binding protein (PBP2a), acquired from another species, which was resistant to the action of the antibiotic 1. Unfortunately, as soon as methicillin was used clinically, methicillin-resistant S. The methoxy groups produced steric hindrance around the amide bond reducing its affinity for staphylococcal β-lactamases. This was achieved in 1959 with the synthesis of methicillin, which had the phenol group of benzylpenicillin disubstituted with methoxy groups ( Figure 1). Efforts were made to synthesise penicillin derivatives that were resistant to β-lactamase hydrolysis. Resistant strains typically produced an enzyme, called a β-lactamase, which inactivated the β-lactam. aureus strains resistant to benzylpenicillin were causing increasing concern. aureus infections before the 1950s involved the administration of benzylpenicillin (penicillin G) ( Figure 1), a β-lactam antibiotic, but by the late 1950s S. aureus can also cause food poisoning, the result of enterotoxin production.
#Pbp3 gene purpose skin#
aureus include, pneumonia, (inflammation of lungs), mastitis (infection of the mammary glands), infections of skin (impetigo, cellulitis and staphylococcal scalded skin syndrome), osteomyelitis (infection of bone), endocarditis (infection of the endothelial lining of the heart and valves) and bacteremia (bacteria present in blood). give rise to toxic shock syndrome leading to fever, sickness and in some cases death.

aureus, where the production of toxins by S. Burns and surgical wound infections are commonly invaded by S. aureus is an opportunist pathogen, and given the right circumstances can cause more serious infections. Healthy individuals are usually unaware of staphylococcal carriage but they may suffer from minor skin infections such as boils and abscesses. aureus on external skin surfaces and the upper respiratory tract, particularly the nasal passages.

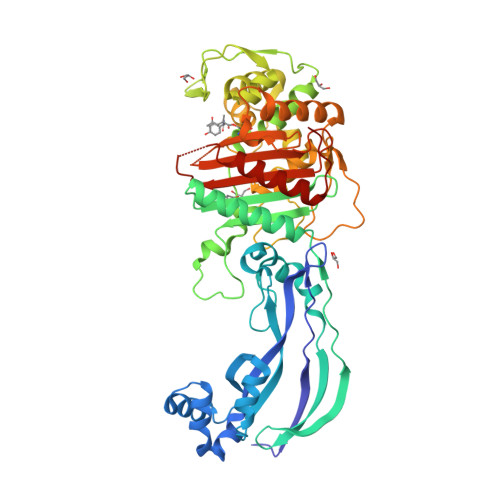
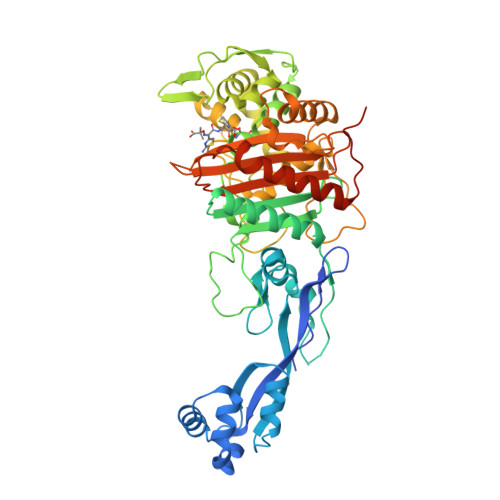
Staphylococcus aureus, a member of the family Micrococcaceae, is a Gram-positive coccus whose cells tend to occur either singly or if dividing cells do not separate, form pairs, tetrads and distinctive irregular “grape-like” structures. Accessory factors, such as Fem factors, provide possible new targets, while compounds that modulate methicillin resistance such as epicatechin gallate, derived from green tea, and corilagin, provide possible lead compounds for development of inhibitors. An understanding of the mechanism of methicillin resistance has led to the discovery of accessory factors that influence the level and nature of methicllin resistance. aureus isolates are often resistant to other classes of antibiotics (through different mechanisms) making treatment options limited, and this has led to the search for new compounds active against these strains. aureus can become resistant to methicillin and other β-lactam antibiotics through the expression of a foreign PBP, PBP2a, that is resistant to the action of methicillin but which can perform the functions of the host PBPs. Methicillin, a β-lactam antibiotic, acts by inhibiting penicillin-binding proteins (PBPs) that are involved in the synthesis of peptidoglycan, an essential mesh-like polymer that surrounds the cell.
Staphylococcus aureus is a major pathogen both within hospitals and in the community.


 0 kommentar(er)
0 kommentar(er)
